Pediatric Obesity Criteria, Does My Child Correspond? Empathizing with Parents’ Anxiety

Pediatric Obesity Criteria, Does My Child Correspond? Empathizing with Parents’ Anxiety
Does our child fall into pediatric obesity criteria? We solve parents’ anxiety together. “Director, our child is tall and has a large frame compared to peers… could it be pediatric obesity? I’m worried because the belly looks a bit more out than kindergarten friends.” This is one of the stories I hear most frequently in the clinic. Many parents come with vague anxiety about their child’s weight. That anxiety often occurs because they do not know exact pediatric obesity criteria well, or even if they know, they are lost on how to cope.
\n\n| \n Once, the mother of 7-year-old Jae-hee (pseudonym) came and asked, “When the child wakes up in the morning, the face is like a `water-soaked sponge`, and she gets exhausted soon even after running just a bit. Could this all be because of obesity?” I deeply empathized with the mother’s worry and explained that it is important to look at the signals the child’s body is sending together. \n |
A child’s weight is not a problem to be judged simply by the number on the scale. Pediatric obesity in the growth period should be approached with a different perspective from adult obesity.
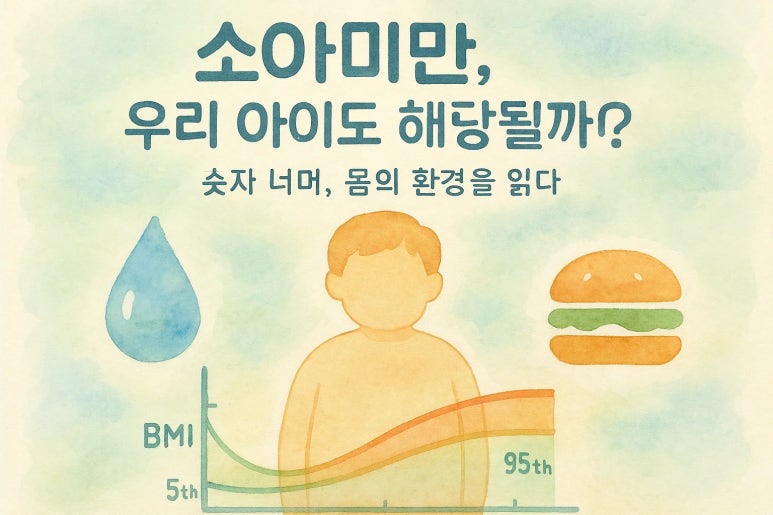
Pediatric Obesity Criteria, Reading the ‘Body Environment’ Beyond Numbers
`Pediatric Obesity Criteria`, shall we look only at numbers? We interpret together with hani-medical context. Pediatric obesity criteria mainly utilize `Body Mass Index (BMI) percentiles` according to age and gender. In the case of children and adolescents aged 2 or older, if BMI is between `85th-95th percentiles`, it is defined as `overweight`, and if `95th percentile` or higher, it is defined as `obese`. This number becomes an important indicator to objectively grasp the child’s current state. However, I try to look more deeply into the `‘body environment’` hidden behind this number.
\n\n| \n I do not see the child’s weight change simply as a problem of calorie intake alone, but interpret it from the perspective of `‘Damp-phlegm’ and ‘Spleen/Stomach function’` hani-medically. ‘Damp-phlegm’ refers to a state where unnecessary water or waste products in our body stagnate as if `the drain of a bathtub is blocked and water doesn’t drain well`. About `70%` of our body consists of water, and as unnecessary surplus stays in the body, it can appear as morning swelling, symptoms of feeling the body is heavy, and strong preference for certain tastes (salty, sweet). Modernly, this can be connected with `body water fluctuation` being large or `salt intake` being high on `BIA (Bioelectrical Impedance Analysis) examination`. `‘Spleen/Stomach function’` is the Zang-Fu that governs digestion, absorption, and metabolism overall, and if `Spleen/Stomach function` is weak, one cannot efficiently utilize nutrients and easily piles up waste products. This often leads to `appetite signal imbalance`, `chronic fatigue`, and `indigestion`. \n |
Such hani-medical perspective complements modern medical indicators and aids more multi-dimensional understanding of our child’s weight problem. For example, even for children of the same `BMI 95th percentile`, the approach should differ between cases where one just ate a lot and cases where one often swells, is lethargic, and digestion is weak so `Damp-phlegm` is accumulated.
\n\n| \n Pediatric obesity is not simply a problem of appearance, but a crucial health problem that can cause `metabolic diseases` such as `precocious puberty`, `hypertension`, and `diabetes`, as well as `growth hindrance`, `learning degradation`, and `psychological shrinkage`. Therefore, a child’s `weight management` can be an important turning point for growth. \n |
Sustainable Pediatric Obesity Management, Wisdom Starting from Small Changes
Sustainable management suitable for our child, how should it start? The most important thing is `‘sustainability’`. It should be a change the child doesn’t get stressed about and the entire family can participate in. Rather than hastily setting goals, it is wise to correct small habits according to the child’s growth speed.
\n\n| \n 10-year-old Min-jun (pseudonym) corresponded to the `obesity criteria` with `BMI` at `96th percentile`. Looking at Min-jun’s meal log, carbohydrate-centered snacks and frequent eating out were problems. Particularly, he had a habit of eating late-night snacks while playing games after dinner. In Min-jun’s case, I confirmed that he has a `constitution where Damp-phlegm easily accumulates` and took correction points as follows. First, he reduced the `Spleen/Stomach burden` by keeping regular meal times to maintain a steady meal interval. Second, he supplemented `protein` with boiled eggs, tofu balls, etc. instead of fruit for snacks, and had `vegetable side dishes` first during meals. Third, the whole family practiced late-night snack prohibition together so he didn’t eat anything within `minimum 3 hours` after dinner. After `3 months`, Min-jun’s `BMI` came down to `90th percentile`, and the biggest change is that he wakes up refreshingly in the morning and activity level increased. Above all, the mother said, “The child gets less irritated than before and the expression has become much brighter.” \n |
Like this, closely observing the child’s constitution and lifestyle habits and starting from small changes suitable for them is the core. The child should never be allowed to handle it alone.
Growth Period Child, Short-term Reduction is Dangerous: Together with an Expert
\n\n
| \n A reckless diet to sharply reduce weight in a short term can have a `fatal impact` on a child’s growth and development. Particularly in the growth period, `muscle mass` should be sufficiently secured for healthy metabolism to occur, and diets only doing `calorie restriction` are highly likely to induce `muscle loss` and incite `yo-yo effects`. Never avoid unverified folk remedies or extreme diets, and be sure to consult with a medical team having professional knowledge about child and adolescent weight management to establish a plan suitable for the child. \n |
Balance Instead of Impatience, a Healthy Growth Path Walking with Your Child
Walking with your child for healthy growth, `find balance` instead of impatience. `Pediatric obesity` starts with numbers, but eventually is a process of looking after the child’s overall health and happiness. I sufficiently understand the vague anxiety felt by novice parents. However, I think this anxiety can be a good opportunity to look closely at the child’s body. Based on accurate information and the help of an expert, `if you healthily cultivate the child’s ‘body environment’`, the quality of life of the whole family as well as the child will improve. Wisdom is needed to `silently walk along according to the child’s speed instead of an impatient mind`. `Meet a medical team that closely looks at the entire body even if it’s not me`. They will be a reliable helper for your child’s healthy growth.